Date: May 28, 2025
By: Bharat Global Time Health Desk
Yes, you read that right. A flesh-eating, heat-resistant fungus is emerging as a potential threat to global health, with scientists warning it could become the trigger for the next pandemic.
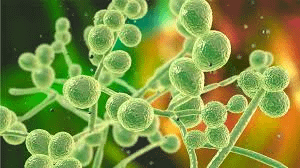
The Fungus in Focus: Candida auris and its Deadlier Cousins
The medical world has been keeping a close eye on Candida auris, a drug-resistant fungal pathogen that has already caused outbreaks in hospitals across the U.S., Japan, India, and Europe.
But recent reports suggest the problem is much larger and much more frightening.
“We are now seeing fungal strains that can survive in human body temperatures, evade antifungal drugs, and—in worst cases—digest human tissue,” said Dr. Ethan Marks, a mycologist at the Global Pathogen Institute.
Some new fungal species discovered in Amazonian soil and melting permafrost appear to thrive in warm environments and exhibit signs of necrotrophic behavior—meaning, they feed on live tissue.
Why This Is So Dangerous
Unlike bacteria and viruses, fungi are eukaryotic organisms, like humans. That means:
- Our immune system finds it harder to detect and eliminate them
- Most antibiotics don’t work—fungal infections need antifungals, which are limited
- Fungal pathogens can mutate rapidly, especially under climate stress
This means a global fungal outbreak would be harder to treat, especially in resource-poor countries.
“We are entering a post-antifungal era,” said Dr. Shreya Malhotra, infectious disease expert at AIIMS, Delhi. “Fungi are adapting faster than our medicines.”
Climate Change: The Breeding Ground
Experts believe climate change is playing a huge role in the rise of these fungi. As the planet warms, fungi are evolving to survive at higher temperatures, which was earlier a barrier to infecting warm-blooded mammals like humans.
“Nature is running simulations,” explains Dr. Thomas Kowalski, a fungal genomics researcher. “The fungi that adapt best to heat and antifungals are now winning the evolutionary race.”
Some strains have already jumped from birds to humans, while others thrive in hospital ICUs, air conditioners, and medical implants—silent, invisible, and deadly.
Symptoms of Infection
Fungal infections like Candida auris start subtly, but can quickly become life-threatening, especially in immunocompromised people.
Watch out for:
- Persistent fever, even after antibiotics
- Skin lesions or wounds that refuse to heal
- Chest infections not responding to treatment
- Neurological symptoms (in extreme brain-invasive cases)
Hospitals may misdiagnose these as bacterial or viral infections, losing precious time.
Are We Ready for a Fungal Pandemic?
Not quite. The world’s medical systems are under-prepared for large-scale fungal outbreaks:
- No vaccines currently exist
- Diagnosis often takes days or weeks
- Only 4 major classes of antifungals exist—and resistance is rising
The WHO has already listed fungal pathogens on its priority watchlist, with Candida auris, Aspergillus fumigatus, and Cryptococcus species at the top.
What Can Be Done?
Health experts are urging:
- Global surveillance networks to track fungal outbreaks
- Stronger regulations on hospital sanitation and air handling
- New investment in antifungal drug research (currently underfunded)
- Public awareness, especially among diabetic and immunocompromised patients
Simple hygiene measures like handwashing, avoiding mold exposure, and not self-medicating antibiotics can reduce fungal spread indirectly.
Final Word
A fungus that can “eat” human flesh sounds like science fiction. But with rising heat, melting ice, and global travel, it may just be science fact in the making. As world health leaders continue to focus on viral threats, the fungal frontier is quietly advancing—and it may already be here.
Stay alert. Stay informed. The next pandemic may not come with a cough—it may start with a rash, a fever… and a fungus





